Peer Reviewed Research Articles
| Article #1 | ||
| Long-term housing subsidies and SSI/SSDI income: Creating health-promoting contexts for families experiencing housing instability with disabilities | ||
| Link: Long-term housing subsidies and SSI/SSDI income: Creating health-promoting contexts for families experiencing housing instability with disabilities – ScienceDirect | ||
| Abstract | ||
| Background: Though disability and housing instability are discussed separately in public health literature, few studies address families at their intersection. As a result, little is known about families who experience both homelessness and disability, how many receive disability benefits like SSI and SSDI, or the influence of those benefits on health-promoting outcomes like housing stability and self-sufficiency. Moreover, no previous research compares the ability of different housing and service interventions to increase disability benefit access. Objective: We examine relationships between disabilities and SSI/SSDI income reported when families enter emergency shelters and later health-promoting outcomes (housing stability and self-sufficiency) and how housing interventions affect SSI/SSDI receipt. Methods: Families in the (name removed) Study (N = 1857) were interviewed in emergency shelters, randomly offered one of three housing interventions or usual care (i.e., no immediate referral to any intervention beyond shelter), and re-interviewed 20 months later.Results: A third of families reported a disability at shelter entry. SSI/SSDI coverage of these families increased nearly 10% points over 20 months but never exceeded 40%. Disabilities predicted greater housing instability, food insecurity, and economic stress and less work and income. Among families reporting disabilities, SSI/SSDI receipt predicted fewer returns to emergency shelter, and more income despite less work. Offers of long-term housing subsidies increased SSI/SSDI receipt. Conclusions: Many families experiencing homelessness have disabilities; those receiving SSI/SSDI benefits have better housing and income outcomes. Providing families experiencing homelessness with long-term housing subsidies and SSI/SSDI could improve public health. Summary: This study highlights how disability, income, and housing instability intersect for homeless families. Many families in shelters include members with disabilities, but most do not initially receive SSI/SSDI benefits. Those who do access disability income tend to have better outcomes, such as reduced shelter reentry and improved financial security. Long-term housing subsidies not only provide immediate shelter stability but also significantly increase the likelihood of families obtaining SSI/SSDI benefits. These findings suggest that coordinated efforts to provide stable housing and streamline access to disability income can improve health and economic outcomes for vulnerable families. |
Article #2
The Effect of Visual Education Aimed at the Basic Needs of Individuals with Disabilities on the Health Literacy and Life Quality of Caregivers
Abstract
| The aim of this research is to evaluate the effect of visual education for the basic needs of people with disabilities on the health literacy and life quality of caregivers. The study sample comprised 268 caregivers evaluated in a pretest-posttest pattern. The data were collected using a Personal Information Form, the Health Literacy Scale, and the World Health Organization [WHO] Life Quality Scale-Short Form. Data were evaluated with the Wilcoxon test and Spearman correlation analysis. Following the education given to caregivers, an increase was determined in the Health Literacy Scale sub-dimension of information comprehension and in the WHO Life Quality Scale-Short Form sub-dimension of social relations. Thus it was seen that the visual education increased the health literacy and life quality of the caregivers. |
Summary
This study highlights the importance of improving health literacy among caregivers of individuals with disabilities, as it directly affects the quality of care and overall well-being of both the caregiver and the person receiving care. It explains that many caregivers struggle with understanding medical instructions, using technology, and managing health tasks, which can lead to repeated hospital visits and poor health outcomes. The research, based on visual education during the COVID-19 pandemic, shows that higher health literacy improves life quality and calls for further studies across diverse populations.
Article #3
| Link: Basic Needs Fulfillment and Course Completion Rates for Online University Students with Disabilities: A Quantitative, Non-Experimental, Causal-Comparative Study | ||
| Abstract | ||
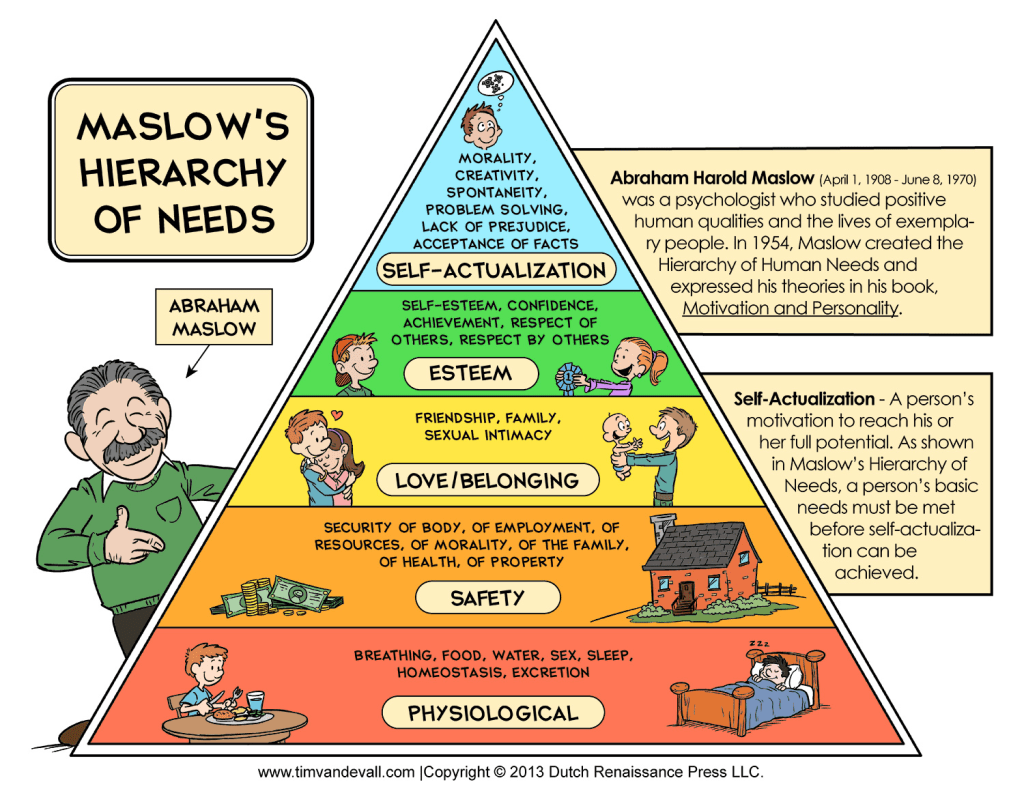
| The purpose of this quantitative, nonexperimental causal-comparative study is to determine if there is a difference in the percentage of courses completed between online university students with disabilities who are experiencing food and/or housing insecurity and those who are not. Students with disabilities at universities are less likely to complete courses than peers without disabilities, and while this discrepancy is often blamed on disability, other factors that impact student performance must be examined to determine if intersecting factors that disproportionately impact people with disabilities, specifically food and housing insecurity, may be contributing to decreased percentages of course completion. The theory guiding this study is Maslow’s Hierarchy of Needs, as it emphasizes the importance of basic psychological needs, such as food and housing, being met in order for people to reach their fullest potential. Research was conducted using the U.S. Household Food Security Survey Module: Six-Item Short Form and the Fragile Families and Childhood Wellbeing 6 Item Housing Questionnaire. Online students at a large university in the Southwest United States of America in a Teachers’ College were surveyed. A random sample of 126 students was used for analysis, taken from 3,031 students surveyed. Data was analyzed using a two-way ANOVA to determine the findings. There were no statistically significant differences in course completion rates between students who were food and housing secure and those who were not. Further research is recommended to understand the impact of food and housing insecurity in both acute and chronic situations for online university students with disabilities. Summary: In this quantitative, non-experimental, casual-comparative study is to determine if there is a difference in the percentage of courses completed between online university students with disabilities who are experiencing food and/or housing insecurity and those who are not. It is to be considered that people with disabilities who experience course incompletion are more likely to face food and housing insecurity. The theory guiding this study is Maslow’s Hierarchy of Needs, as it emphasizes the importance of basic psychological needs, such as food and housing, being met in order for people to reach their highest potential. Research was conducted using the United States household food Security Service. A random sample of 126 students was used for analysis, taken from 3031 students surveyed. Students with disabilities are most likely to live in poverty areas and lack healthcare and other valuable resources including their basic needs being met. The finding also showed no difference of students who attended online courses or on campus with needs of food and housing insecurity have a high rate of not completing their courses. Article #4 Are They the Same for All People? Nurses’ Knowledge about the Basic Human Needs of People with Disabilities Link: Are They the Same for All People? Nurses’ Knowledge about the Basic Human Needs of People with Disabilities – PMC Abstract Nursing care involves a continuous interaction between nurses and people with disabilities. This has created a need for assessment tools that measure nurses’ knowledge about the basic human needs of people with disabilities. The aim of this cross-sectional study was to develop a Knowledge of Basic Human Needs Scale and investigate nurses’ levels of knowledge about the basic human needs of people with disabilities and their association with nurses’ education. Data were analyzed using principal component analysis to test the construct validity and to identify factors using principal varimax rotation. The reliability estimate was based on Cronbach’s alpha coefficient. Linear regression models were used to assess the association between knowledge about basic human needs and predictors. Factor analysis extracted eight factors, explaining 66.3% of the total variance. The sampling adequacy, criterion validity, and internal consistency were satisfactory. The nurses’ levels of education was associated with their knowledge about the basic human needs of people with disabilities. The questionnaire constitutes a valuable contribution to improving nurses’ knowledge and practice, as well as the quality of healthcare, and it provides a contribution to improving the quality of life for people with disabilities. Summary: The article, published in January 2023, focuses on the vital role nurses play in caring for individuals with disabilities. Nurses are often the first point of contact in hospitals, and the quality of care they provide can significantly impact whether the needs of these individuals are met. Studies suggest that nurses with more education, experience, and knowledge, especially those with master’s degrees, are more aware of the basic human needs of people with disabilities, as defined by Maslow’s Hierarchy of Needs: physiological, safety, love and belonging, esteem, and self-actualization. When any of these needs go unmet, individuals with disabilities may struggle. With over one billion people worldwide living with a disability, nurses must recognize how long-term impairments interact with societal barriers to limit access to necessary care. The article emphasizes that health cannot be fully achieved without addressing these foundational needs. A study tested nurses of varying ages, education levels, and experience using tools to measure their awareness and ability to meet the needs of people with disabilities. Despite a few limitations, the results showed strong reliability and validity, reinforcing the importance of proper training. The findings confirmed that increasing knowledge among healthcare professionals, particularly nurses, is essential to improving health outcomes for people with disabilities. Article #5 Entrenched Opportunity: Medicaid, Health Systems, and Solutions to Homelessness. Link: Entrenched Opportunity: Medicaid, Health Systems, and Solutions to Homelessness. Abstract Context: As inequality grows, politically powerful health care institutions-namely Medicaid and health systems-are increasingly assuming social policy roles, particularly related to solutions to homelessness. Medicaid and health systems regularly interact with persons experiencing homelessness who are high users of emergency health services and who experience frequent loss of or inability to access Medicaid services because of homelessness. This research examines Medicaid and health system responses to homelessness, why they may work to address homelessness, and the mechanisms by which this occurs. Methods: The authors collected primary data from Medicaid policies and the 100 largest health systems, along with national survey data from local homelessness policy systems, to assess scope and to measure mechanisms and factors influencing decision-making. Findings: Nearly one third of states have Medicaid waivers targeting homelessness, and more than half of the 100 largest health systems have homelessness mitigation programs. Most Medicaid waivers use local homelessness policy structures as implementing entities. A plurality of health systems rationalizes program existence based on the failure of existing structures. Conclusions: Entrenched health care institutions may bolster local homelessness policy governance mechanisms and policy efficacy. Reliance on health systems as alternative structures, and implementing entities in Medicaid waivers, may risk shifting homelessness policy governance and retrenchment of existing systems. Summary: This article talks about how Medicaid and big health systems are starting to take on a bigger role in addressing homelessness, especially because the usual systems in place, like Continuums of Care (CoCs), which are mostly nonprofit groups, haven’t been very effective. The authors explain that health systems and Medicaid are powerful and well funded, so they’re in a better position to help. The article highlights that many states now have Medicaid waivers focused on homelessness, and over half of the largest health systems have programs to help unhoused people. These programs usually offer support like housing navigation, behavioral health care, and sometimes even help with rent or shelter. A lot of this change happened after the Affordable Care Act, which expanded Medicaid access and encouraged connections between health care and housing support. The study also found that while some Medicaid programs work with local homeless service groups, others rely more on hospitals or health systems to lead. There are challenges though, like administrative barriers, lack of coordination, and Medicaid rules that make it hard for homeless people to keep their coverage. Even so, some hospitals are stepping in because they see how homelessness leads to more ER visits, higher costs, and worse health outcomes. Overall, the article says this shift could help improve care and reduce homelessness, but only if it is done thoughtfully. It also warns that if health systems take over too much, they might push out local experts who actually understand homelessness best. |